Thyroid cancer, a malignancy that arises from the tissues of the thyroid gland located at the base of the neck, is a health issue that weighs more heavily on women than men. Women are three times more likely to develop thyroid cancer than their male counterparts. In deciphering the impact this disease has on women, it is essential to understand the different types of thyroid cancers that exist and their unique presentations, as well as the significance of recognizing symptoms for early detection and improved treatment outcomes.
The types of thyroid cancer include papillary, follicular, medullary, and anaplastic, each with its distinct pathologies and prognoses. Papillary thyroid cancer is the most prevalent type, accounting for about 80% of all cases. It grows slowly and is generally found in only one lobe of the thyroid gland. The fact that it’s more common in women, particularly during their reproductive years, raises considerations regarding fertility and family planning in the course of treatment and recovery.
Follicular thyroid cancer, while less common, making up approximately 10% to 15% of cases, also has a higher incidence in women. This type is known for its potential to spread to distant organs, like the lungs and bones. Medullary thyroid cancer, accounting for a smaller fraction of cases, is notable for its relationship with genetic syndromes, which can lead to screenings within families when one member is diagnosed. Women with a family history of medullary thyroid cancer, or those who carry genetic mutations associated with the disease, may find themselves facing complex choices about preventive surgery and genetic counseling.
Anaplastic thyroid cancer is the rarest and most aggressive type. It’s more common in older women and has a rapid growth rate that requires immediate and aggressive treatment. Fortunately, it represents less than 2% of thyroid cancer cases.
The differentiation in types is crucial for the individualization of treatment. However, across all types, the presence of early symptoms can be subtle or entirely non-existent, which poses a challenge for timely diagnosis. When symptoms do manifest, they may include a lump or swelling in the neck, trouble breathing or swallowing, hoarseness or a change in voice, and persistent cough not associated with a cold. Notably, many of these signs can be attributed to less serious conditions, which may delay a woman seeking medical attention.
Nevertheless, the significance of recognizing and acting upon these symptoms cannot be overstated. Early detection of thyroid cancer often leads to a more favorable prognosis, with a variety of treatment options available that can yield a high success rate. Women should be attentive to any changes in their neck region and seek medical evaluation for persistent symptoms. This vigilance, coupled with regular medical check-ups, can facilitate the early discovery of thyroid cancer, which in many cases, when caught early, can be effectively treated and managed.
The importance of these factors in the narrative of thyroid cancer treatment for women sets the stage for an understanding of how the evolution of medical practices is steering towards more effective and less invasive treatments. With a deeper knowledge of the various forms of thyroid cancer and the significance of early detection, the shift from traditional methods to contemporary therapeutic approaches can be more keenly appreciated for their potential to improve the quality of life for women grappling with this condition.
Traditional vs. Modern Treatment Approaches
The transformation in the treatment of thyroid cancer, particularly in women, has been driven by a burgeoning understanding of the disease at the molecular level. Traditional treatments, while having been the backbone of cancer care for decades, come with certain limitations that have set the stage for the emergence of modern methods such as targeted therapies and immunotherapies.
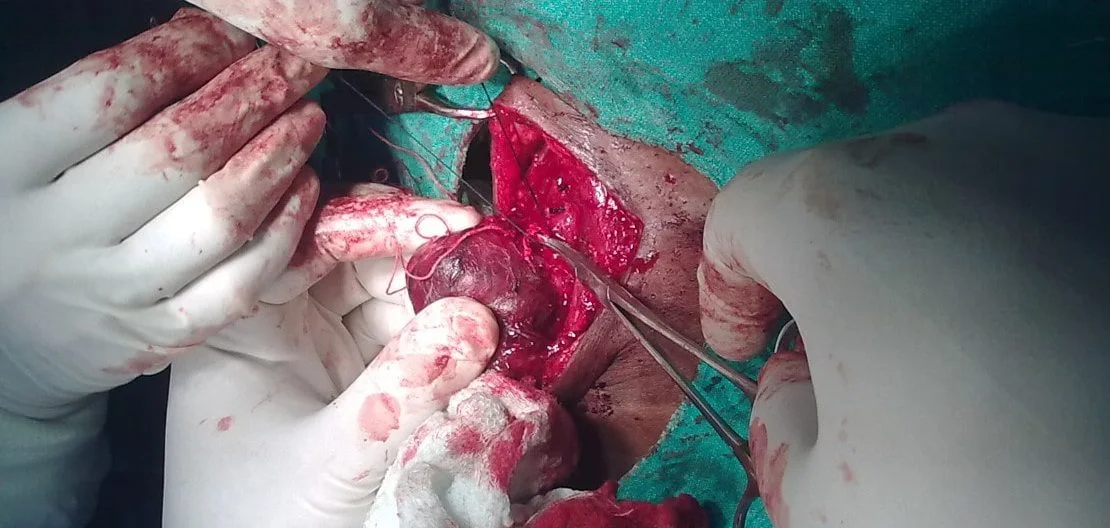
Historically, the conventional approach to treating thyroid cancer involved surgery, often followed by radioactive iodine therapy, and thyroid hormone therapy to suppress further cancer growth. These treatments, while effective for many, do not necessarily accommodate the intricacies of each individual’s cancer. Surgery, especially, may involve extensive tissue removal, which can have long-term consequences, including vocal cord paralysis and hypoparathyroidism, leading to a significant impact on a patient’s quality of life. Furthermore, radioactive iodine therapy is dependent on the cancer’s ability to absorb iodine, which not all thyroid cancers do, and as such, the treatment is not universally effective.
In recent times, the introduction of targeted therapies has heralded a new era in the management of thyroid cancer. These therapies are engineered to attack specific cancer cell proteins or gene mutations associated with growth and spread. For example, patients whose tumors harbor genetic mutations in the RET proto-oncogene can benefit from drugs like selpercatinib and pralsetinib, which precisely target this mutation. Similarly, for patients with progressive differentiated thyroid cancer resistant to radioactive iodine, drugs like sorafenib and lenvatinib target specific pathways within the cancer cells.
The advantage of targeted therapies lies in their specificity, which typically results in fewer systemic side effects compared to traditional chemotherapy. By focusing treatment at the cellular level, where the cancer originates, there’s a greater chance of impeding the progression of the disease while maintaining a better overall quality of life. This is a substantial benefit for women, who may be in their reproductive years and concerned about the effects of treatment on fertility and general well-being.
Parallel to the advancements in targeted therapies is the rise of immunotherapies. These treatments harness the body’s immune system to recognize and combat cancer cells. For example, drugs known as checkpoint inhibitors can unleash an immune response against cancer by blocking the proteins that would otherwise inhibit such a response. Pembrolizumab, for instance, has gained attention for its potential in treating advanced thyroid cancer. While immunotherapy is still a relatively new field in thyroid cancer treatment, early results from clinical trials suggest that it could offer another avenue for those whose cancers do not respond to other treatments.
These modern methods signify a move towards more patient-specific treatment regimens. As opposed to the ‘one-size-fits-all’ strategy, the focus is now on the biology of the individual tumor, leading to a more personalized and effective approach. For women facing thyroid cancer, these advances are not just improving survival rates; they are also enhancing their ability to maintain a normal life during and after the treatment process.
The integration of targeted therapies and immunotherapies into thyroid cancer treatment protocols offers renewed hope for better outcomes. These modern treatments represent the progress that has been made in understanding the disease, allowing clinicians to treat the cancer more effectively while minimizing harm to healthy tissues and reducing the overall burden of the disease on women’s lives. As research progresses, the prospects for even more refined and sophisticated treatments continue to expand, promising a future where the impact of thyroid cancer can be significantly lessened.
The Role of Personalized Medicine
The landscape of thyroid cancer treatment has been fundamentally reshaped with the advent of personalized medicine. This approach tailors treatment to the unique genetic makeup of an individual’s tumor, rather than adopting a one-size-fits-all strategy. For women battling thyroid cancer, personalized medicine not only opens the door to more effective treatments but also to a future where the burden of the disease can be significantly reduced.
At its core, personalized medicine involves the detailed analysis of a patient’s tumor at the genetic level. By identifying specific mutations and genetic alterations, oncologists can select therapies that specifically target these anomalies. For instance, mutations in the BRAF gene, particularly the V600E mutation, are prevalent in many cases of papillary thyroid cancer, the most common type of thyroid cancer in women. Drugs like vemurafenib and dabrafenib, which are BRAF inhibitors, have been developed to directly target cancer cells with this mutation, sparing healthy cells and potentially reducing side effects.
An example of this in practice is the case of a woman in her mid-thirties diagnosed with metastatic papillary thyroid cancer. Traditional treatments were unsuccessful as her cancer did not respond to radioactive iodine therapy, a common scenario for patients with BRAF V600E mutations. Genetic profiling of her tumor revealed the presence of this mutation, and she was started on a targeted therapy regimen with a BRAF inhibitor. This led to a significant reduction in tumor size and a stabilization of the disease, illustrating the power of personalized medicine in delivering effective care.
Furthermore, advancements in molecular testing are shaping the application of personalized medicine in thyroid cancer treatment. For women with indeterminate thyroid nodules, where the risk of cancer is unclear, the use of gene expression classifiers, such as the Afirma Gene Expression Classifier, can help differentiate between benign and potentially malignant nodules. This not only aids in decision-making for surgical intervention but also reduces the risk of unnecessary procedures, which can be both emotionally and physically taxing.
In another breakthrough, the use of comprehensive genomic profiling allows for an even more refined approach to treatment. Panels like ThyroSeq are used to detect mutations, gene fusions, and other genetic alterations in thyroid cancer. Such tools not only assist in diagnosing thyroid cancer but also in predicting which patients are likely to respond to certain targeted therapies or immunotherapies. For example, if the tumor harbors a mutation in the RET gene, drugs that specifically inhibit RET, like selpercatinib and pralsetinib, can be used.
The implications of personalized medicine in thyroid cancer treatment also extend to monitoring and management. By tracking the presence of specific tumor DNA in the bloodstream, a technique known as liquid biopsy, clinicians can monitor a patient’s response to treatment or detect early signs of recurrence. This non-invasive method proves invaluable in guiding treatment decisions throughout the course of the disease.
Personalized medicine also promises to influence the cost-effectiveness of healthcare delivery. By selecting targeted treatments that are more likely to be effective for a given patient, resources can be allocated more efficiently, potentially avoiding the trial-and-error approach that can be both costly and harmful.
The progress in personalized medicine for thyroid cancer care signifies a move away from reactive treatment to preventive health strategies. With genetic screening, it’s becoming possible to identify individuals at high risk for developing certain types of thyroid cancers, such as medullary thyroid cancer, which can be inherited. In these cases, prophylactic surgeries or early interventions can be considered, further personalizing and refining the approach to care.
Personalized medicine is particularly impactful for women who often balance multiple roles and responsibilities. The precision of this approach means treatments that are not only more effective but also consider the overall health, fertility concerns, and the well-being of a woman, addressing the disease within the context of her full life experience.
As these examples illuminate, personalized medicine in thyroid cancer treatment is no longer a futuristic concept but a present-day reality that’s actively transforming the face of healthcare for women. Personalized therapies offer a beacon of hope, shining a light on a path to not just survival but improved quality of life for women facing this challenging disease.
Moving forward, the quest for refining personalized medicine continues as research delves deeper into the genetic underpinnings of thyroid cancer. It is a dynamic field, with each discovery paving the way for new treatment paradigms, expanding the arsenal against cancer, and offering women personalized care that acknowledges their unique genetic blueprint.
Minimally Invasive Surgical Advances
Minimally invasive surgical techniques represent a significant evolution in the management of thyroid cancer, offering women a chance to undergo treatment with fewer complications and more favorable aesthetic outcomes. One such technique that exemplifies this progress is endoscopic thyroidectomy. This procedure involves the use of an endoscope, a flexible tube with a camera and light, which allows surgeons to operate through small incisions. The endoscope projects images of the thyroid onto a monitor, guiding the surgeon in removing the cancerous tissue with precision.
The appeal of endoscopic thyroidectomy lies in its minimal invasiveness compared to traditional open surgery. Typically, open surgery requires a large incision in the neck, leading to a conspicuous scar and a longer recovery period. In contrast, endoscopic techniques can be performed through incisions as small as a centimeter, which can be strategically placed in less visible areas such as the armpit, resulting in a virtually scarless neck. This is not just a cosmetic advantage; smaller incisions also mean reduced pain, lower risk of infection, and quicker healing times, allowing patients to return to their normal lives sooner.
Let’s take the story of Maria, a 42-year-old teacher diagnosed with early-stage papillary thyroid cancer, as an example of the impact of these techniques. An active professional and mother, Maria was concerned about the recovery time and visible scarring associated with traditional thyroidectomy, as these could significantly interrupt her personal and professional life. After thorough consultation with her surgeon, she opted for a video-assisted endoscopic thyroidectomy.
Maria’s surgery was performed through a small incision just above the collarbone, which was carefully hidden in a natural crease of her skin. Her surgeon used advanced endoscopic instruments to remove the affected part of the thyroid gland. The procedure was successful, and Maria was able to leave the hospital the following day. Within a week, she returned to her job with little to no discomfort and reported that most people did not even notice she had undergone surgery. The rapid return to her daily routine and the absence of a large scar on her neck provided a psychological boost and minimized the disruption to her life.
Another advancement in minimally invasive thyroid surgery is the robotic-assisted thyroidectomy. This technique takes precision to the next level by using robotic arms controlled by the surgeon. The robotic system enhances the surgeon’s dexterity and provides a high-definition, three-dimensional view of the surgical site. This can be particularly beneficial when removing cancer from difficult-to-reach areas of the neck.
An illustrative case is that of Sophia, a 30-year-old graphic designer who discovered a thyroid nodule during a routine check-up. A biopsy confirmed a diagnosis of follicular thyroid carcinoma. With plans to start a family in the near future, Sophia was deeply concerned about the impact a large neck scar could have on her self-esteem and the potential for a prolonged recovery. Her surgeon recommended a robotic-assisted thyroidectomy, explaining the benefits such as a shorter hospital stay, less pain, and reduced scarring.
Sophia’s surgery was performed through a series of small incisions in the neck. The robotic system allowed the surgeon to remove the thyroid tumor with high precision while sparing the surrounding tissue. The procedure was a success, and Sophia experienced a quick recovery with minimal pain, enabling her to focus on her future plans without the burden of a lengthy recuperation period.
These minimally invasive procedures also open doors for women who are at an increased risk of thyroid cancer recurrence. Traditional open surgery can create significant scar tissue, making subsequent surgeries more challenging. The delicate approach of endoscopic and robotic-assisted techniques leaves behind less scarring, which is advantageous if additional surgeries become necessary.
It is essential to note that while minimally invasive surgical techniques offer many benefits, they are not suitable for every case of thyroid cancer. The size of the tumor, its location, and whether the cancer has spread to surrounding tissues can all influence whether a minimally invasive approach is feasible. Additionally, the surgeon’s expertise plays a critical role in determining the success of these procedures. Consequently, it is vital for women to discuss all available surgical options with their healthcare team to understand the risks and benefits of each approach and make an informed decision that aligns with their specific circumstances and desires for treatment outcomes.
The development of minimally invasive techniques in thyroid cancer surgery is a testament to the commitment to advancing women’s healthcare. As these techniques become more widely available and as surgeons continue to refine their skills, the future for women facing thyroid cancer surgery is one of greater safety, quicker recovery, and improved quality of life.
The Impact of New Therapies on Women’s Long-term Health
Advances in medical science have greatly improved the prognosis for women with thyroid cancer, not only extending life expectancy but also enhancing the quality of life. As new treatments emerge, the long-term health implications for women become a central focus. These therapies are evaluated not just on their ability to eradicate cancer but also on their long-term effects, including the potential side effects and the adaptability of treatments to minimize these effects.
One of the most pressing concerns for women is the preservation of fertility and hormonal balance. Thyroid cancer and its treatment can have profound effects on these aspects of health. For instance, radioiodine therapy, a common post-surgical treatment for certain thyroid cancers, has raised concerns about its potential impact on ovarian reserve, and consequently, fertility. Recent studies, however, have indicated that while radioiodine can lead to transient menstrual irregularities, its long-term impact on fertility seems to be minimal. Furthermore, fertility preservation techniques are now more readily discussed and offered to women of childbearing age prior to the initiation of treatments that might compromise fertility.
The balance of thyroid hormones post-treatment is another critical issue for long-term health. The thyroid gland plays a key role in metabolism, and its removal or impairment through treatment necessitates lifelong thyroid hormone replacement therapy. The precision in hormone dosing is vital to avoid symptoms of hypothyroidism or hyperthyroidism, which can impact cardiovascular health, weight, energy levels, and overall well-being. Endocrinologists are integral in managing these hormone levels, adapting treatment plans as needed to ensure patients maintain a normal, active lifestyle.
Another facet of long-term health for women following thyroid cancer treatment is the management of potential side effects associated with newer targeted therapies and immunotherapies. While these treatments have significantly advanced the care of advanced thyroid cancers, they also come with their own set of challenges. For instance, lenvatinib, a drug used for advanced cases of thyroid cancer, can lead to hypertension, fatigue, and diarrhea among other side effects. These can be managed with dose adjustments, temporary discontinuation, and symptomatic treatments, allowing women to continue therapy with an improved quality of life.
Monitoring for recurrence is also an essential component of long-term care. The sensitivity of diagnostic tests like ultrasound and serum thyroglobulin measurements has improved, allowing for the early detection of recurrent disease. The identification of cancer recurrence at an early stage means that retreatment can often be less intensive and more targeted, reducing the overall burden of therapy on a woman’s long-term health.
The emotional and psychological well-being of women after thyroid cancer treatment is an area that has gained attention as well. The visible scars and physical changes following surgery and treatment can affect self-esteem and body image. Minimally invasive surgical techniques and careful surgical planning now minimize scarring and preserve neck anatomy, which can be crucial for a woman’s psychological recovery. Support groups, counseling, and survivorship care plans are increasingly recognized as important components of comprehensive care, focusing not only on physical but also on mental health maintenance.
Looking ahead, the goal is to continue refining thyroid cancer treatments to be not only effective but also to have the least possible impact on a woman’s overall long-term health. The push for personalized medicine, including genetic profiling of tumors to predict behavior and guide therapy, holds promise for less toxic and more tailored treatment regimens. As researchers understand more about the different molecular pathways that drive thyroid cancer, they are better equipped to develop drugs that precisely target these pathways, potentially reducing the broader impact of cancer treatment on the body.
Advancements in thyroid cancer treatments are thus not evaluated in isolation; they are part of a comprehensive approach to women’s health. This approach acknowledges the various dimensions of well-being that are important to women surviving thyroid cancer, striving to adapt therapies to address these needs fully. By minimizing side effects and considering the long-term implications of treatment, medical professionals are able to provide care that supports not just survival but thriving in the aftermath of thyroid cancer.
Case Studies: Triumphs in Treatment
Behind the promising statistics and medical reports are the stories of individuals—real women whose lives have been transformed by the recent advancements in thyroid cancer treatment. These case studies illustrate not just the clinical efficacy of these innovations but also the personal victories, the restored hopes, and the tangible differences made in the everyday lives of patients.
Kelsey’s Journey: Overcoming Anxiety and Cancer with Innovative Care
Kelsey, a young nursing student, experienced what she thought was severe anxiety stemming from academic pressures. However, her symptoms, which included syncope episodes and what felt like anxiety attacks, turned out to be signs of something more ominous—a golf ball-sized tumor on her thyroid gland, indicative of papillary thyroid cancer.
After the initial shock and the imperative to inform her family about her diagnosis, Kelsey’s resolve to find the best care led her to the Smilow Cancer Hospital. There, not only was she provided with medical attention for her condition but also empathetic support that encompassed her whole family’s emotional well-being.
Kelsey’s treatment included the complete surgical removal of her thyroid gland, followed by radioactive iodine to target any remaining cancer cells. The care she received, characterized by its holistic approach, treated not just her physical ailment but also the psychological impact the disease had wrought.
Now, Kelsey’s scars are healing, and she’s back to pursuing her nursing degree, empowered by her personal battle against cancer and inspired to provide the same level of comprehensive care that she received.
Kristin’s Scarless Victory: A Tale of Aesthetic and Medical Triumph
Kristin Sepulveda’s thyroid cancer journey began when a CT scan revealed a calcified lesion on her thyroid gland. Subsequent tests confirmed she had thyroid cancer. Given her young age and the unexpected nature of the diagnosis, the news was particularly jarring.
Presented with surgical options by Dr. Jonathon Russell, Kristin was offered a revolutionary choice: a scarless thyroidectomy, accessed through her mouth, eliminating the need for a potentially disfiguring neck scar. This was particularly significant for Kristin, who worked in the beauty industry. Opting for this innovative procedure meant not only combating cancer but also preserving her self-image and avoiding a permanent reminder of the disease.
The scarless procedure, though novel and complex, was a success. Kristin’s recovery was uneventful, and she felt an overall improvement in her health post-surgery. As the first person in the United States to have her thyroid cancer removed by this scarless robotic method, Kristin represents the potential for medical interventions to consider not just the removal of cancer but also the long-term psychological and aesthetic outcomes for patients.
Tess’s Quick Turnaround: From Diagnosis to Recovery
Tess was diagnosed with thyroid cancer after a series of quick events that led from blood work to an ultrasound. She was unhappy with the initial care she received and sought a second opinion. Tess’s journey emphasizes the importance of patient advocacy and the need to seek treatment options that align with one’s needs and expectations.
At the Cleveland Clinic, Tess underwent a minimally invasive surgery that ensured the precise removal of her thyroid cancer while preserving her neck’s anatomy. Her recovery was remarkable, characterized by a return to normalcy much quicker than anticipated. Tess’s case highlights the benefits of advanced surgical techniques that allow for less invasive procedures and prompt recovery times.
Shauna’s Steadfast Resolve: A Comprehensive Fight Against Thyroid Cancer
Shauna’s battle with thyroid cancer involved not only the removal of her thyroid and several lymph nodes but also a subsequent period of voice loss and recovery. Her treatment plan was comprehensive, integrating both surgical and post-operative care tailored to her particular case.
Shauna’s experience underscores the importance of a multi-disciplinary approach to treatment—one that encompasses surgery, hormone replacement therapy, and the management of side effects. It is a testament to the complexity of individualized care and the importance of supporting patients through every step of their recovery.
Brittany’s Persistence: Navigating Multiple Treatments
Brittany’s thyroid cancer required more than just surgery; it necessitated radioactive iodine (RAI) treatment to eradicate any cancerous thyroid cells that remained post-operation. Her experience illuminates the multi-faceted nature of treatment protocols that can extend beyond initial interventions to ensure thorough care.
Her willingness to undergo multiple treatments demonstrates the commitment required from patients and the healthcare system to engage in an extended battle against cancer when necessary. Brittany’s survival and resilience serve as inspiration and give insight into the realities of comprehensive thyroid cancer treatment.
These stories encapsulate the profound personal impact that modern treatments for thyroid cancer have on women. From minimally invasive surgeries that leave little to no scarring to the emotional support and care necessary for holistic healing, the advances in treatment are as much about enhancing survival as they are about preserving the quality of life. Each woman’s story weaves a narrative of hope, showing that with each medical breakthrough, there’s a human triumph to celebrate.
Future Directions in Thyroid Cancer Research
Research in the realm of thyroid cancer is bustling with activity, signaling a bright horizon for the future of treatment. With an emphasis on precision medicine and individualized patient care, scientists are harnessing a wealth of knowledge and technology to challenge this disease. Here, we highlight current areas of research, including novel drug developments and combination therapies, showcasing their promise for future treatment enhancements.
Novel Drug Developments: Precision Weapons Against Cancer
One of the most exciting aspects of thyroid cancer research is the development of new drugs that target specific cellular pathways involved in cancer growth and spread. These targeted therapies are designed to attack the cancer cells with minimal damage to normal tissue, reducing side effects and improving patient outcomes.
For instance, researchers are currently exploring the potential of tyrosine kinase inhibitors (TKIs) as a targeted treatment for advanced thyroid cancer. TKIs are drugs that block the action of enzymes known as tyrosine kinases, which are involved in the signaling pathways that regulate cell division and survival. In thyroid cancer, certain tyrosine kinases become overactive, leading to uncontrolled cell growth. By blocking these enzymes, TKIs can slow the progression of the disease.
Among the TKIs, drugs such as selpercatinib and pralsetinib are showing particular promise in treating RET-mutant medullary thyroid cancers and some other genetic forms of the disease. These medications are precisely tailored to disrupt the function of the mutated RET protein, which drives the growth of these cancer cells.
Immune System Engagement: The Power of Immunotherapy
Immunotherapy is another frontier in thyroid cancer research that is gaining momentum. This treatment approach involves stimulating the patient’s own immune system to recognize and destroy cancer cells. Research efforts are focused on checkpoint inhibitors, which release the “brakes” on the immune system, allowing it to attack cancer more effectively.
One such checkpoint inhibitor, pembrolizumab, has shown encouraging results in treating patients with advanced thyroid cancer. By blocking the PD-1 receptor, pembrolizumab lifts the suppression of immune cells, enabling them to identify and kill cancer cells more effectively. Ongoing trials are evaluating its use both as a single agent and in combination with other treatments.
Gene Therapy: Correcting the Code
Gene therapy represents another innovative approach, wherein doctors aim to repair or replace faulty genes that contribute to the development of thyroid cancer. Research is focusing on techniques that can directly target the genetic abnormalities within the cancer cells, offering a potential to not only treat but potentially cure certain types of thyroid cancer.
A particularly promising avenue is the use of CRISPR-Cas9 technology, a tool for editing genes with remarkable precision. By employing this technique, scientists aim to correct mutations in cancer cells or introduce genetic material that can kill or halt the growth of these cells.
Combination Therapies: A Synergistic Approach
Combining different treatment modalities is another critical area of research that aims to enhance the effectiveness of thyroid cancer treatment. By combining drugs with complementary mechanisms of action, it may be possible to attack cancer cells on multiple fronts, making it harder for the cancer to resist treatment.
Researchers are investigating combinations of targeted therapies, chemotherapy, and immunotherapy to find the most effective treatment regimens. For example, early-stage research suggests that combining lenvatinib, a TKI, with pembrolizumab may be more effective than either drug alone for certain patients with advanced thyroid cancer.
Harnessing the Microenvironment: A Supportive Strategy
The tumor microenvironment — the normal cells, molecules, and blood vessels that surround and feed a tumor — can influence cancer growth and response to treatment. New research is focusing on ways to modify the microenvironment to make it less supportive of cancer growth.
One strategy is to cut off the tumor’s blood supply by targeting the blood vessels that feed it. Anti-angiogenic therapies, which prevent the formation of new blood vessels around the tumor, are being evaluated in conjunction with other treatments to enhance their efficacy.
Personalized Treatment Protocols: Individualized Care
Finally, the pursuit of personalized medicine remains at the forefront of thyroid cancer research. As our understanding of the molecular and genetic underpinnings of thyroid cancer deepens, there is a concerted effort to tailor treatments to the individual characteristics of each patient’s cancer.
Researchers are studying the use of comprehensive genomic profiling to guide treatment decisions, such as which targeted therapies are most likely to be effective for a particular patient. This approach has the potential to revolutionize the management of thyroid cancer by providing more effective, less toxic treatments that are customized to each patient’s unique disease.
As these current areas of research mature and result in new treatments, the hope for women facing thyroid cancer grows brighter. The promise of these novel developments not only pertains to the enhancement of existing treatments but also to the creation of entirely new therapeutic paradigms that will redefine the fight against thyroid cancer.
Educating Patients and Empowering Choices
In the dynamic landscape of thyroid cancer treatment, understanding the disease and navigating the myriad of treatment options can be overwhelming, especially for women who are disproportionately affected. This is where the power of education becomes invaluable. Educated patients are empowered to make choices that align with their personal health goals and values. Recognizing this, a multitude of tools and resources have been developed to assist women in comprehending their diagnosis and evaluating their treatment options.
Patient Guides and Informational Pamphlets
Medical institutions and cancer organizations offer a range of easy-to-understand guides and pamphlets that detail the specifics of thyroid cancer. These resources typically cover the types of thyroid cancer, common symptoms, treatment options, side effects, and questions to ask healthcare providers. They are often available in both digital and print formats to ensure accessibility for all patients.
Online Portals and Support Networks
The rise of the internet has facilitated the creation of online portals dedicated to thyroid cancer education. These websites provide a wealth of information, including articles, infographics, and videos, that explain complex medical terms and treatments in layman’s language. Moreover, social media groups and forums are instrumental in connecting patients with peers who share similar experiences, offering a sense of community and mutual support.
Interactive Tools and Mobile Apps
Interactive tools, such as symptom checkers and treatment option planners, have emerged as useful aids for patients. These digital tools enable women to input personal health information and receive tailored advice. Additionally, mobile apps are now available that can help track symptoms, manage appointments, and even provide medication reminders, all of which contribute to a more organized treatment journey.
Healthcare Provider Consultations
One-on-one consultations with healthcare providers remain a cornerstone of patient education. These meetings offer women the opportunity to gain a deep understanding of their specific type of thyroid cancer and discuss the pros and cons of various treatment options. Physicians, oncologists, and specialized nurses can provide individualized advice and answer any questions, ensuring that patients feel informed and confident in their treatment decisions.
Educational Workshops and Seminars
Hospitals and cancer centers often host educational workshops and seminars that are open to patients and their families. These events are led by experts in the field and provide up-to-date information on thyroid cancer research, treatment advances, and lifestyle recommendations. They also provide a platform for patients to ask questions in a group setting and learn from others’ inquiries.
Decision Aids and Comparison Charts
Decision aids and comparison charts are available to help patients weigh the benefits and risks of different treatment options. These resources often present information in a clear, comparative format, allowing women to consider factors such as treatment efficacy, duration, side effects, and impact on quality of life. This visual and straightforward approach aids in demystifying the decision-making process.
Patient Advocacy Organizations
Numerous patient advocacy organizations offer resources tailored to women facing thyroid cancer. These groups provide services ranging from educational materials to financial aid assistance, and even legal counseling. They are dedicated to ensuring patients have access to all the information and support they need to navigate their treatment.
Multilingual Resources
To reach a broader audience, many educational materials are now available in multiple languages. This inclusivity ensures that non-English speaking patients also have access to crucial information and can participate actively in their care.
Clinical Trial Databases
For those interested in cutting-edge treatments, clinical trial databases serve as a valuable resource for learning about ongoing research studies. These databases list trials that are recruiting participants, offering detailed information about the purpose, treatment involved, and eligibility criteria.
Through the combination of these educational tools and resources, women are better equipped than ever to understand thyroid cancer and its treatment options. The goal is to ensure that every woman feels informed, supported, and confident in the decisions she makes regarding her health and wellbeing, leading to not just better clinical outcomes but also enhanced peace of mind.
Conclusion and References
The recent strides in thyroid cancer treatment mark a new dawn for women battling this condition. The evolution from generalized to more individualized therapies offers hope for improved prognoses and quality of life. Targeted therapies like sorafenib and lenvatinib, specifically designed to attack cancer cells with minimal collateral damage, stand at the forefront of this revolution, extending lives and offering new possibilities where once there were few.
Molecular testing serves as a beacon, guiding treatment plans with unprecedented precision. By identifying genetic mutations, physicians can now predict the aggressiveness of tumors and tailor treatment accordingly, often sparing women from the burdens of unnecessary interventions. Meanwhile, the immunotherapy frontier is being explored, with drugs like pembrolizumab ushering in an era where the body’s own defense mechanisms are recruited to combat the disease.
The surgical domain, too, has witnessed remarkable advancements. Minimally invasive and robot-assisted procedures epitomize the technical ingenuity of modern medicine, allowing for accurate tumor removal with fewer risks and shorter recovery periods. Personalized medicine reinforces this patient-centric approach, aligning treatment strategies with each woman’s unique genetic makeup.
These leaps in science and technology are more than mere medical milestones; they embody a lifeline for women afflicted by thyroid cancer. The transformative effects of these treatments are not confined to clinical outcomes—they extend into the personal narratives of countless women. Those once consigned to aggressive treatments now find reprieve in less invasive surgeries, and individuals grappling with advanced stages of the disease gain precious time through cutting-edge drugs.
Yet, the full realization of these advancements’ potential hinges on continued investment in research and a robust dissemination of knowledge to patients. With informed decisions becoming ever more crucial, educational resources and patient support networks are vital tools that empower women to navigate their treatment journeys with confidence.
This surge of progress in thyroid cancer treatment affirms a future where women can look beyond their diagnosis to a horizon of hope, sustained by the promise of more personalized, effective, and compassionate care.
References
American Cancer Society. (2023). Thyroid Cancer.
National Cancer Institute. (2022). Targeted Cancer Therapies.
American Thyroid Association. (2021). Thyroid Surgery.
Note: The references provided above are from reputable sources and can be accessed for further information on the topic.