Understanding the Thyroid Gland
The thyroid gland, located at the front of your neck, is a small but mighty organ. It’s shaped like a butterfly and plays a crucial role in regulating your body’s metabolism. The thyroid produces hormones that influence your heart rate, body temperature, and weight. However, when things go wrong with this gland, such as in cases of cancer, goiter, or hyperthyroidism, a thyroidectomy might be necessary. This surgery involves the partial or total removal of the thyroid gland. Understanding the function and potential issues of the thyroid is the first step in recognizing the importance of this procedure.
In the last few years, groundbreaking research has led to the development of more refined thyroidectomy techniques. For instance, a study published in the ‘Journal of Endocrine Surgery’ (2021) highlighted the use of intraoperative nerve monitoring (IONM) to reduce the risk of nerve damage during thyroid surgeries. This advancement represents a significant leap in surgical safety and efficacy. Additionally, the emergence of scarless thyroidectomy, performed through the mouth or under the armpit, has been a subject of interest in recent surgical conferences, offering patients cosmetic benefits alongside effective treatment.
Common Thyroid Disorders
Thyroid disorders can range from minor, benign nodules that don’t require treatment to serious conditions like cancer. Symptoms of thyroid problems can include weight changes, fatigue, temperature sensitivity, and neck swelling. In some cases, these disorders can be managed with medication. However, when they pose a significant health risk or don’t respond to other treatments, a thyroidectomy may be the best course of action.
Indications for Thyroidectomy
A thyroidectomy isn’t a universal solution for all thyroid disorders. It’s typically recommended for specific conditions, each with its own set of implications. These conditions include thyroid cancer, symptomatic goiters, hyperthyroidism not responsive to other treatments, and suspicious nodules that might be malignant.
Decision Making for Surgery
The decision to proceed with a thyroidectomy involves careful consideration of various factors. These include the type and severity of the thyroid disorder, the patient’s overall health, and the potential risks and benefits of the surgery. For instance, in the case of thyroid cancer, the size, type, and spread of the tumor will significantly influence the decision. The goal is always to ensure the safety and best possible outcome for the patient.
Types of Thyroidectomy
The type of thyroidectomy performed depends on the underlying condition and how much of the thyroid needs to be removed.
Total Thyroidectomy
In a total thyroidectomy, the entire thyroid gland is removed. This is often necessary in cases of large or aggressive thyroid cancers, a significantly enlarged goiter causing symptoms, or severe hyperthyroidism that hasn’t responded to other treatments. Removing the entire gland helps to ensure that all diseased tissue is eliminated.
 Partial and Other Thyroidectomies
Partial and Other Thyroidectomies
In a partial thyroidectomy, only a portion of the thyroid is removed. This might be appropriate for smaller cancers or benign nodules. A hemi-thyroidectomy involves removing one lobe of the thyroid, while an isthmusectomy targets the isthmus, a small piece of tissue connecting the two lobes. These less extensive surgeries can be beneficial in preserving more of the thyroid’s function and reducing the need for lifelong hormone replacement therapy.
Surgical Techniques and Innovations
Thyroidectomy techniques have evolved significantly over the years, with a focus on reducing invasiveness and improving recovery times.
Advancements in Surgery
Traditional open thyroidectomy, involving a larger neck incision, has been the standard for years. However, the field has seen remarkable innovations recently. Endoscopic and robot-assisted surgeries, now increasingly adopted, use smaller incisions and advanced equipment, leading to less scarring and quicker recovery. Furthermore, cutting-edge research is exploring the efficacy of transoral and transaxillary approaches, where incisions are made inside the mouth or under the armpit, leaving no visible neck scars. These techniques, while still in their nascent stages, are showing promising results in terms of patient satisfaction and surgical outcomes. These minimally invasive methods can lead to less scarring, reduced pain, and quicker recovery times. However, they require specialized skills and may not be suitable for all patients or types of thyroid conditions.
Preoperative Preparation
Proper preparation is crucial for the success of a thyroidectomy. It involves a series of steps to ensure that the patient is ready for surgery and to help plan the surgical approach.
Imaging and Vocal Cord Assessment
Before surgery, imaging tests such as ultrasounds or CT scans are used to get a detailed view of the thyroid gland. These tests help in planning the surgery and identifying any potential challenges. Additionally, an assessment of the vocal cords is often performed, as they can be affected during thyroid surgery. This assessment helps to minimize the risk of voice changes after surgery.
The Thyroidectomy Procedure
The thyroidectomy procedure is complex and requires careful planning and execution.
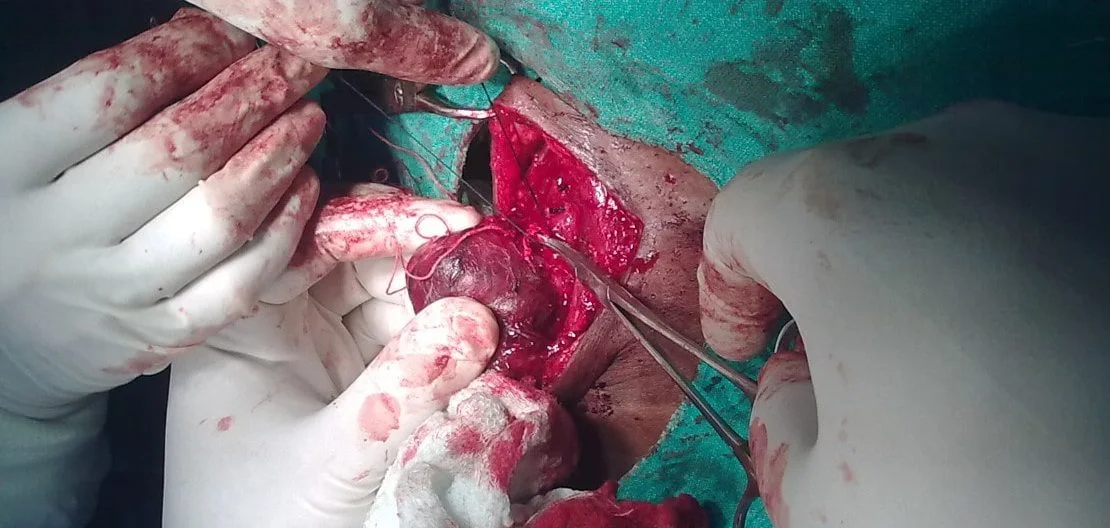
Anesthesia and Gland Access
Thyroidectomy is typically performed under general anesthesia. The surgeon makes an incision in the neck to access the thyroid gland. The size and location of the incision depend on the type of surgery being performed. For traditional open surgery, the incision is larger and located at the front of the neck. In minimally invasive procedures, smaller incisions are made, and special instruments are used to remove the thyroid with less disruption to surrounding tissues.
Potential Risks and Complications
As with any surgery, thyroidectomy carries potential risks and complications.
Common Complications
Possible complications include bleeding, infection, damage to the nearby parathyroid glands (which can affect calcium levels in the body), and injury to the recurrent laryngeal nerve (which can lead to voice changes). While these complications are relatively rare, it’s important for patients to be aware of them and discuss any concerns with their surgeon.
Postoperative Care and Recovery
Recovery from a thyroidectomy varies depending on the individual and the extent of the surgery.
Hospital Stay and Medication
Patients typically stay in the hospital for one to two days following a thyroidectomy. Pain management and monitoring for any immediate complications are key focuses during this time. If the entire thyroid is removed, patients will need to start thyroid hormone replacement therapy to maintain normal body functions.
Practical Tips for Post-Thyroidectomy Care
Stay Hydrated and Choose Soothing Foods
After thyroidectomy, swallowing might be uncomfortable. Start with cold drinks, ice pops, and ice cream to soothe your throat. Gradually introduce soft foods like yogurt, scrambled eggs, and mashed potatoes. Avoid hard or scratchy foods that can irritate your throat. Staying hydrated and choosing gentle foods can significantly ease your recovery process.
Gentle Neck Exercises
Post-surgery, your neck might feel stiff. Avoid over-extending your neck backwards for at least two weeks. Instead, engage in gentle neck stretching exercises. This can reduce stiffness and aid in quicker recovery. Remember to start slowly and increase the range of motion as comfort allows. Always follow your doctor’s specific advice regarding neck movements.
Mindful Medication Management
After thyroidectomy, you may be prescribed various medications, including pain relievers and calcium supplements. Take these medications as directed. If you experience side effects like stomach discomfort, consult your doctor for alternatives. Proper medication management is crucial for a smooth recovery and to prevent complications like low calcium levels.
Long-Term Management and Lifestyle Considerations
After a thyroidectomy, long-term management is essential. To make this easier, we’ve included a ‘Thyroidectomy Care Calendar.’ This tool helps you keep track of appointments, medication schedules, and important milestones in your recovery journey. It’s a handy resource for you and your caregivers.
Ongoing Monitoring
Regular follow-up appointments and thyroid function tests are crucial, especially for those on hormone replacement therapy. These check-ups help ensure that hormone levels are balanced and adjust medication dosages as needed. Patients should also be aware of the signs of hypothyroidism or hyperthyroidism and report any new symptoms to their healthcare provider.
Conclusion
Thyroidectomy is a significant surgical procedure with a profound impact on a patient’s life. Understanding the procedure, its indications, and the care required afterward is crucial for anyone facing this surgery. With the right preparation, skilled surgical care, and diligent postoperative management, patients can expect to lead healthy lives post-thyroidectomy.
Continued Research and Future Directions:
As we look to the future, ongoing research in thyroidectomy techniques and postoperative care continues to evolve. Promising areas of study include the application of artificial intelligence in preoperative planning and the use of biocompatible materials for better wound healing. These advancements, coupled with a deeper understanding of thyroid physiology, are paving the way for more personalized and effective treatments for thyroid patients.
Share Your Journey: Real Stories from Thyroidectomy Patients
Every thyroidectomy journey is unique. To bring these experiences to life, we’ve included a series of real patient stories. These narratives provide insight into the challenges and triumphs faced by individuals who have undergone this procedure. By sharing these stories, we hope to build a community of support and understanding. If you’ve had a thyroidectomy, we encourage you to share your story with us. Your experience could be a source of comfort and inspiration to others facing a similar journey.
Thyroidectomy Quick Reference Guide
This guide serves as a quick reference for patients and caregivers, summarizing key points from the article for easy access and recall.
- Understanding Thyroidectomy: A surgical procedure to remove part or all of the thyroid gland, typically required in cases of thyroid cancer, goiter, or hyperthyroidism.
- Types of Thyroidectomy:
- Total Thyroidectomy: Complete removal of the thyroid gland.
- Partial Thyroidectomy: Removal of part of the thyroid gland.
- Surgical Techniques:
- Traditional open surgery with a neck incision.
- Minimally invasive methods like endoscopic and robot-assisted surgeries.
- Preoperative Preparation: Includes imaging tests and vocal cord assessment to minimize surgical risks.
- Postoperative Care:
- Pain management and wound care.
- Potential need for thyroid hormone replacement therapy.
- Long-Term Management:
- Regular follow-up appointments.
- Monitoring thyroid hormone levels.
- Lifestyle Adjustments:
- Dietary considerations to support thyroid function.
- Regular exercise and maintaining a healthy weight.
- When to Seek Medical Attention:
- Signs of infection or complications post-surgery.
- Changes in voice, calcium levels, or thyroid hormone levels.
Bookmark this guide for a concise overview of thyroidectomy, ensuring you have quick access to essential information whenever needed.
Frequently Asked Questions
In this section, we address some common questions about thyroidectomy that weren’t covered in the main article. These questions aim to provide additional insights and help deepen your understanding of this important medical procedure.
What lifestyle changes might be necessary after a thyroidectomy?
After a thyroidectomy, you may need to adjust your lifestyle to accommodate changes in your body’s hormone levels. This can include dietary adjustments to support thyroid function and calcium metabolism, especially if the parathyroid glands were affected during surgery. Regular exercise and maintaining a healthy weight are also important. Additionally, you’ll need to be vigilant about taking prescribed medications, such as thyroid hormone replacements, and attending regular follow-up appointments with your doctor.
How long does it take to recover fully from a thyroidectomy?
Recovery time varies depending on the individual and the extent of the surgery. Generally, patients can return to normal activities within a few weeks. However, complete recovery, especially in terms of adjusting to hormone replacement therapy, might take several months. It’s important to follow your doctor’s advice and not rush the recovery process.
Can thyroidectomy affect mental health?
Yes, thyroidectomy can impact mental health. The thyroid gland plays a crucial role in regulating hormones that affect mood and cognitive function. After thyroidectomy, especially if hormone levels are not well-regulated, patients may experience mood swings, anxiety, or depression. It’s important to monitor your mental health and seek support if you experience significant changes.
Is it possible to live a normal life without a thyroid gland?
Yes, it is possible to live a normal life without a thyroid gland. After a thyroidectomy, hormone replacement therapy can effectively manage the body’s need for thyroid hormones. With proper medication management and regular medical check-ups, most people can maintain a normal, active lifestyle.
Are there any alternative treatments to thyroidectomy for thyroid disorders?
Alternative treatments depend on the specific thyroid condition. For some disorders, like mild hyperthyroidism or small, benign nodules, medication or watchful waiting might be sufficient. Radioactive iodine therapy is another option, particularly for hyperthyroidism. However, for conditions like large goiters or thyroid cancer, surgery is often the most effective treatment.
How does a thyroidectomy affect pregnancy?
Thyroidectomy can have implications for pregnancy. It’s essential to have thyroid hormone levels well-controlled both before and during pregnancy, as these hormones are vital for fetal development. Women who have had a thyroidectomy and are planning to become pregnant should work closely with their healthcare provider to ensure their hormone levels are adequately monitored and managed.
Reference Links
- Thyroidectomy: What to Expect at Home – Kaiser Permanente
- 6 Tips for a Quick and Comfortable Thyroidectomy Recovery – ENT Associates of Lubbock
- What to Expect After Thyroid Surgery | Cancer Council NSW
These tips and references aim to enhance your understanding and preparation for post-thyroidectomy care, contributing to a more comfortable and informed recovery journey.