Ovarian cysts are common in many women of childbearing age. However, scary as that sounds, not all ovarian cysts are bad, or dangerous. Nor do they adversely affect fertility. In fact, most cysts related to estrus ‘function’ are quite natural. The follicles your ovaries produce each month for instance are actually small cysts.
Ovarian Cysts
Ovarian cysts vary in type, size, and consistency depending on their cause.
Types Of Ovarian Cysts
Ovarian cysts can be loosely categorized as ‘functional cysts’ and ‘non-functional cysts’.
Functional cysts are harmless
Functional cysts arise as part of estrus ‘function’ so are more common in childbearing-age women. They’re usually benign cysts that resolve with time and rarely cause fertility problems.
- Follicular cysts: develop when a follicle doesn’t rupture and release its egg (ovulation process) during an estrus cycle but keeps growing. They may also develop when a mature follicle collapses before rupturing. Most follicular cysts disappear naturally.
- Corpus luteum cysts: once a follicle has ruptured and released its egg into the fallopian tubes, it shrinks and begins secreting progesterone and estrogen. This is its corpus luteum phase, designed to prepare the uterus for pregnancy. Sometimes however the egg’s exit hole gets blocked and the follicle fills with fluid instead.
- Hemorrhagic ovarian cyst: can be mistaken for an ectopic pregnancy. Caused when blood vessels in follicles and corpus lutea hemorrhage and fill it with blood. If these cysts rupture, they can be very painful and lead to hemoperitoneum and sepsis if not treated.
Non-Functional Cysts
Non-functional cysts can cause significant health issues and adversely affect fertility. They’re also not part of a normal menstrual cycle so are the more common types of cysts seen in menopausal and post-menopausal women.
- Dermoid cysts: typically develop during child-bearing years but can also arise in older women. They occur when an unfertilized egg begins spontaneously dividing into different cell types – bone, hair, muscle, fat, and even teeth. Exactly what triggers this is not yet understood.
- Cystadenoma: these develop on the internal epithelial tissue lining of an ovary. Most are benign and rarely affect fertility. They can however get very big and rupture or cause ovarian torsion. They usually require surgical treatment. There are several types of cystadenomas:
- Serous cystadenomas: filled with clear thin fluid.
- Mucinous cystadenomas: contain mucin, a jelly-like substance. If they rupture, it can cause a pseudomyxoma peritonei (PMP).
- Endometriomas: contain endometrial tissue, a rich blood-filled tissue that normally lines the uterus. Endometriosis is the abnormal growth of endometrial tissue outside the uterus. It can grow in the ovaries, and result in endometriomas (chocolate-colored cysts). Endometriomas may reach grape-fruit size.
In the US, over 10% of reproductive-age females have endometriosis. - Clear cell cystadenoma is a clear fluid-filled sac, most often associated with endometriosis. They are not common and are often found incidentally during a pelvic exam or PAP smear.
- Seromucinous cystadenoma contain a mix of serous and mucinous fluids, and may also be associated with endometriosis.
All these cysts require intervention if they threaten uterine health.
 Risk Factors For Ovarian Cysts
Risk Factors For Ovarian Cysts
Some things increase the risk of developing ovarian cysts, including:
- Endometriosis
- Infertility treatment – clomiphene citrate, a fertility drug used to induce ovulation, increases corpus luteum cyst development in around 10% of women treated with it.
- Pregnancy
- Hormone therapy
- Polycystic ovary syndrome
Endometriosis, Ovarian Cysts And Fertility Concerns
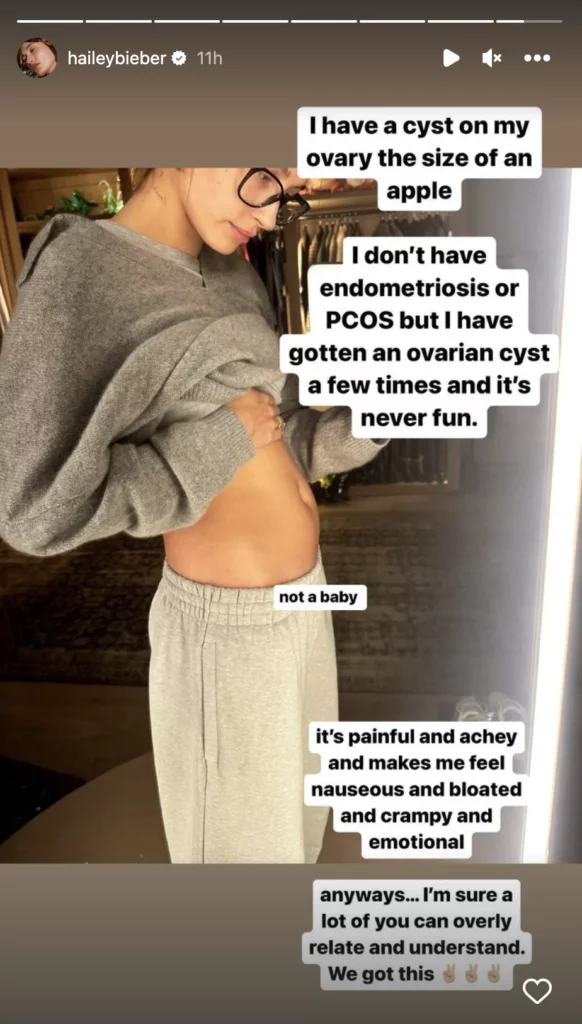
A cyst usually won’t affect fertility and make it harder to get pregnant. However, if an underlying condition like endometriosis is causing them, you may well experience fertility issues and have problems falling pregnant naturally.
Also, in the case of cancer or severe cysts, both ovaries or the uterus may have to be removed.
Dermoid Cysts
Most dermoid cysts are benign but around 1 – 2% turn malignant. They can however grow large enough to block blood flow or cause uterine torsions so are usually surgically removed.
Polycystic Ovaries
‘Polycystic’ means ‘many cysts.’ Women with this condition (around 30%) have many immature follicles or small cysts that fail to mature and produce viable eggs. However, having polycystic ovaries dosen’t always mean polycystic ovary syndrome (PCOS).
For a diagnosis of PCOS, there must be several conditions present.
Polycystic Ovary Syndrome
Polycystic ovary syndrome is a complex hormonal condition diagnosed by the presence of at least 2 of 3 of the following:
- oligo/anovulation (irregular/absent periods)
- hyperandrogenism: high levels of androgens (male hormones), hirsutism (excessive male pattern body/facial hair), scalp alopecia, and acne,
- a polycystic ovary
D ue to these conditions, many women with PCOS also suffer from:
ue to these conditions, many women with PCOS also suffer from:
- reduced fertility and difficulty falling pregnant due to poor ovulation rate,
- obesity,
- insulin resistance (affects 80% of females with PCOS),
- increased risk of Type 2 diabetes (impaired glucose tolerance),
- depression, anxiety, and mood swings,
- hypertension,
- sleep apnoea.
The cause of PCOS is unknown, but hormones, lifestyle, and family history and genetics are all thought to play a role.
PCOS Treatment Options
Management options for PCOS involve:
- A healthy lifestyle with more exercise and a balanced diet,
- Weight loss if overweight (even 5-10% weight loss can significantly improve outcomes),
- Medical treatments to help reduce hormonal imbalances: hormonal birth control pills, infertility drugs, male hormone-blocking medications,
- Iinsulation sensitivity medication,
- Llaser treatment to destroy male hormone producing tissues and resolve hormonal imbalance,
- Counseling
Ovarian Cysts – What To Look Out For
Most women unknowingly develop a cyst in one ovary or both ovaries during their lives. They rarely cause symptoms severe enough to warrant medical attention however. In fact, as per the US Office on Women’s Health, only around 8% of childbearing-age women will develop one big enough to require medical treatment or surgical removal.
They also share some symptoms with early pregnancy so can be overlooked.
Nevertheless, if a cyst ruptures, or blocks blood flow, it may mimic ovarian cancer, causing:
- Sudden changes to the menstrual cycle ie very light, very heavy, or irregular periods
- Unusual bleeding or spotting
- Pelvic pain and sudden pain in the lower abdomen and/or back pain
- Abdominal discomfort such as heaviness/bloating
- Appetite loss
- A feeling of fullness after only small amounts of food
- Frequent/urgent urination
- Difficulty emptying the bladder or bowels
- Painful sex
- Vomiting or fever
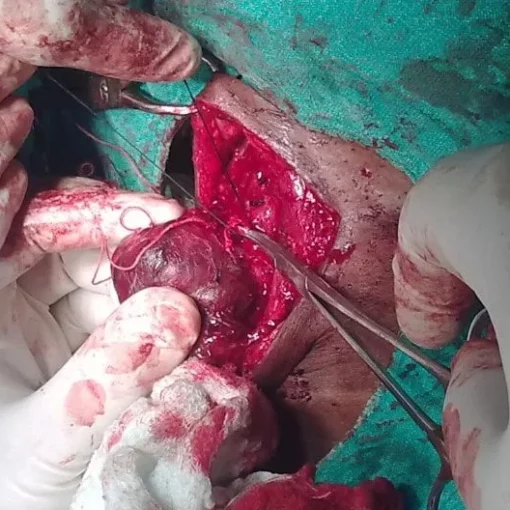
Ovarian Cyst Removal
If a CT scan finds large, cancerous, twisted, ruptured, or painful cysts, they are usually removed by surgery. As the likelihood of developing a cancerous cyst increases with age, older patients are more likely to require surgery. The type of ovarian cyst dictates the procedure used ie laparoscopic or open surgery.
During laparoscopic surgery, a laparoscope is inserted through a small incision in the lower abdomen to locate and remove the ovarian cyst.
Large ovarian cysts are removed via open surgery with general anesthesia. Note however that even after an ovarian cyst is removed, a new cyst may develop.
If there is no cancer, complications are unlikely and recovery only takes a few weeks. If cancer is found, the affected ovary or ovaries may need to be removed and cancer therapy started.
Surgery to remove ovarian cysts may cause fever, chills, abdominal swelling, vomiting, pain, or bleeding. Call your doctor if you experience any of these after your operation.
In Summary:
Most ovarian cysts heal on their own and aren’t a concern. However, seek medical attention immediately if you experience severe ovarian cyst symptoms.